Abstract
Background: Common acute manifestations of sickle cell disease (SCD), including vaso-occlusive pain episodes (VOE) and other complications, are often treated in the emergency department (ED). Effective treatment in the ED remains challenging and often only includes supportive care, such as analgesics and intravenous (IV) fluids. There is clinical equipoise regarding the type of IV fluid to use for resuscitation, and while normal saline (NS) is the most commonly one used in the ED, some SCD providers discourage use of NS. Patients with SCD and kidney dysfunction, who are often at-risk for acidosis already, may not effectively excrete the high sodium, hyperosmolar load of NS, and in large volumes NS may cause hyperchloremic metabolic acidosis that could impact sickle red blood cell (sRBC) rheology (Nath, Nat Rev Nephrol, 2015). We recently demonstrated modestly hyperosmolar and acidotic fluids like NS (308mOsm/L, pH=5.5) may dehydrate sRBCs, increase sRBC/endothelium adhesion, and worsen deformability; and we also showed NS bolus use in pediatric pain management in the ED was associated with inferior pain control, increased likelihood of hospital admission, and more time spent in the ED (Carden et al., Blood & AJH, 2017&2019). Rigorous studies examining the impact of IV fluids, particularly NS, during ED management of adults with SCD have not been performed, and recent evidence suggests that balanced crystalloids (B) may be safer for resuscitation of adults in the ED.
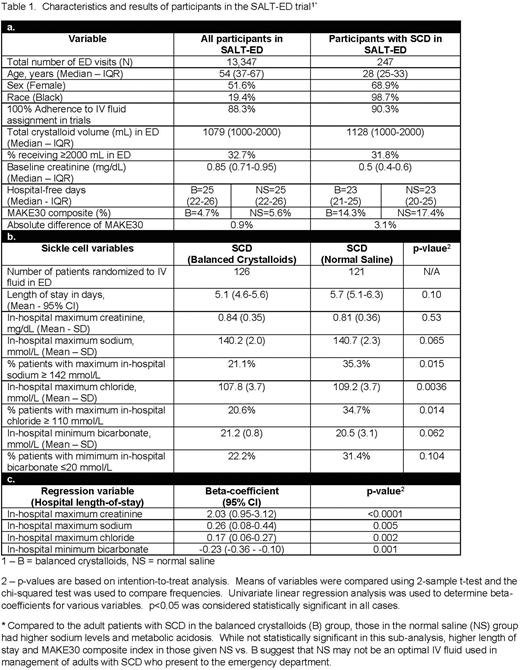
Methods: We utilized data from the seminal SALT-ED study, a single-center, pragmatic, multiple-crossover prospectively randomized controlled trial (RCT) that compared outcomes related to administration of balanced crystalloids (primarily lactated ringers [LR], 274mOsm/L, pH=6.5) to NS administration to all-comer adult patients in the ED (Self et al., NEJM, 2018). Using ICD-10 codes, we conducted an intention-to-treat sub-analysis of SCD patients in the SALT-ED trial. Enrolled participants were non-critically ill adults (18 years and older) with SCD who presented to the ED and were subsequently hospitalized to a non-ICU bed at the hospital. Chief complaint was captured when available. The primary outcome examined was median hospital free days post-index hospitalization and secondary outcomes included a composite of adverse kidney events and death (i.e. MAKE30), as well as changes in serum electrolyte status.
Results: There were 150 adults with SCD identified in the SALT-ED study (Table 1a). Of 13,347 visits captured, 247 ED visits were attributed to these 150 patients - N=126 visits (51%) in the B group and N=121 (49%) in the NS group. Over 50% of documented chief complaints in the ED were pain-related. Compared to all adult patients in the SALT-ED study, those with SCD were younger, more likely to identify as female and Black, have a lower baseline creatinine, and while having similar hospital free days and similar volumes of crystalloids administered in the ED, patients with SCD had an approximate 3.5 times higher odds of suffering an acute kidney injury event (i.e. MAKE30 endpoint) during hospitalization. Compared to those with SCD randomized to the B group, those patients with SCD in the NS group had more adverse kidney events, increased mean length of hospital stay, higher maximum in-hospital sodium, higher maximum in-hospital chloride, and lower minimum in-hospital bicarbonate, suggesting an increased risk of high sodium acidosis with NS use in the ED (Table 1a&b). Using combined data from both groups and analyzing with linear regression, we found in-hospital electrolyte levels were significantly associated with hospital length of stay among adults with SCD administered IV fluids in the ED (Table 1c).
Conclusion: The results from this large RCT sub-analysis further support recent evidence suggesting NS is not an ideal resuscitation IV fluid for adults with SCD presenting to the ED with pain and other complications. Adult patients with SCD randomized to NS in the ED had higher rates of in-hospital high sodium levels, metabolic acidosis, increased hospital stay, and increased kidney events. Our findings suggest that administering balanced crystalloids like LR may be a better option for IV fluid resuscitation among adults with SCD presenting to the ED. Further research is needed to confirm these findings and to determine the optimal IV fluid regimen for adults with SCD presenting to the ED with VOE or other complications.
Disclosures
Carden:Forma Therapeutics, Inc: Current Employment, Current equity holder in publicly-traded company. Lebensburger:Agops: Consultancy; BPL: Consultancy; Forma Therapeutics, Inc: Consultancy; Novartis: Consultancy. Derebail:Bayer: Consultancy; Pfizer: Consultancy; Forma Therapeutics, Inc: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal